Complete Orthodontic and Orthognathic Surgery Course
Course by: Bill Arnett
Duration: 22 Hours
This course is a comprehensive presentation of diagnosis and treatment planning for surgeons, orthodontists, and prosthodontists. The goals of comprehensive treatment include facial balance, airway enlargement, and bite correction. This course facilitates the goals of treatment by examining the essentials of care including, general patient history, TMJ diagnosis and stabilization, facial analysis and treatment, facial and airway cephalometrics, model analysis, orthodontic preparation, 2D and 3D computer diagnosis and treatment, and surgical techniques and tricks for excellence.
EXTRACT FROM THIS COURSE:
WHAT WE COVER IN THIS COURSE:
1.Introduction to Orthodontics and Surgery
- What is our philosophy of treatment?
- What are protocols for treatment?
- How are outlines used to improve lecture comprehension?
- How is lecture retention maximized?
- Are forms part of teaching orthodontics and surgery?
2. Evolution of Orthognathic Surgery and Orthodontics
- How have orthodontics and surgery changed?
- Has the indication for bite treatment changed over 40 years?
- Is crowding resolution different today than in the past?
- Is open joint surgery on the rise or on the decline?
- Is surgery done first or after orthodontics? Trends?
- Why are we definitely trending towards counterclockwise surgery?
- How has profile planning changed over 40 years?
3. Goals of Treatment
- Why do we treat patients? What is supposed to be the end result?
- What are the six goals of orthodontic and surgical treatment?
- Do we achieve these goals?
- Can treatment cause complications?
- What 2 forms are used to explain treatment to the patients?
4. General Patient History
- What forms are used to reveal important patient information?
- What four factors motivate patients to undergo treatment?
- What is the patient motivation for treatment form?
- Does the general patient history form reveal patients who will be impossible to satisfy?
5. TMJ Examination (Analysis)
- What are functional and dysfunctional TMJ remodeling?
- Does bite treatment cause condylar remodeling?
- Has literature been published to explain condylar resorption?
- What TMJ history questions are important?
- What form is used for clinical TMJ analysis?
- What form is used to examine CBCT?
- What CBCT findings predict bite treatment will relapse?
- What blood tests reveal TMJ instability?
6. TMJ Stabilization - Part 1
- What are key disc, muscle, and joint change questions?
- What important factors describe the shape, cortex, and position of the TMJ?
- Does TMJ remodeling create surgical, orthodontic, and prosthetic relapse?
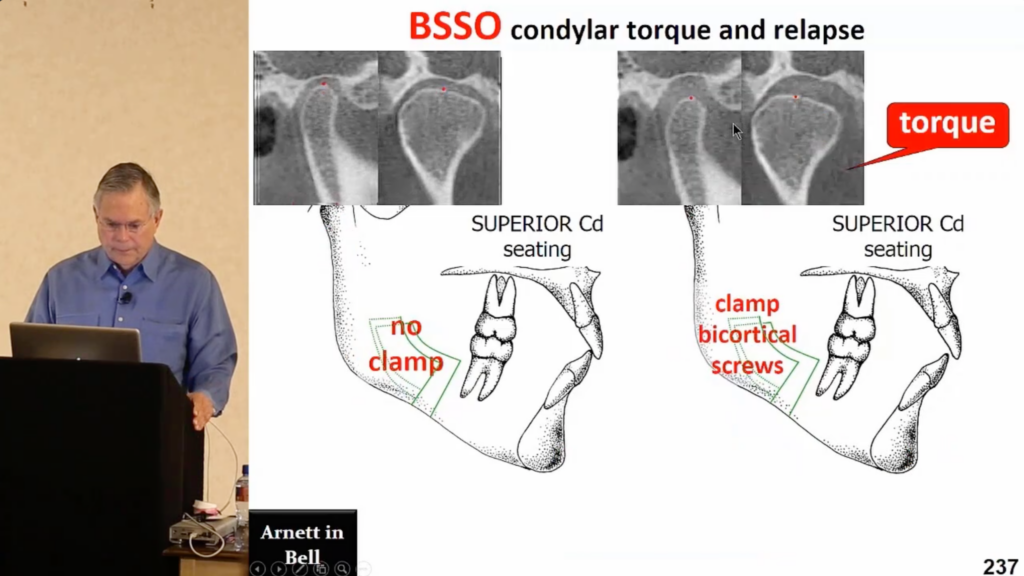
- How do condylar torque, bruxism, and low vitamin D cause condylar resorption and mandibular relapse?
- What publications have described medical management of the TMJ?
- Is late mandibular relapse secondary to condyle position change during surgery?
7. TMJ Stabilization - Part 2
- What surgical techniques are associated with late relapse?
- How do bicortical screws cause late relapse of the mandible?
- How does the medial pterygoid muscle affect relapse?
- Is a long BSSO or short BSSO split desired and why?
- What is done presurgery, during surgery, and after surgery to stabilize the TMJ?
- Do medications control bite correction relapse?
- Do splints stabilize or injure the TMJ?
8. Large Mandibular Advancement Cases
- Can large mandibular advancements be stable? How?
- What is done presurgically to stabilize the TMJ?
- What is done during surgery to stabilize the TMJ?
- What is done after surgery to stabilize the TMJ?
- Does the literature indicate that miniplates have better stability than bicortical screws?
9. Facial Analysis – Part 1
- How should the profile be planned?
- Is there a form to guide analysis of the facial profile?
- What are the essential profile facial traits that guide bite treatment?
- What is the upper lip mirror test?
- What factors influences upper lip projection?
- What 6 factors determine chin projection?
- Does flattening the occlusal plane increase chin projection and throat length?
- Does the face mimic the TMJs?
- What is important facial information?
10. Facial Analysis – part 2
- What 4 techniques do doctors use to plan the face?
- Why do cranial base cephalometrics (Steiner, Ricketts, etc.) misdiagnose dental and skeletal positions?
- Is there a form to guide frontal facial analysis?
- How should the frontal face be planned?
- What are the essential frontal facial traits that guide bite treatment?
- What four factors determine upper incisor exposure under the lip?
- What are the 3 options for leveling the maxillary canines?
- What 3 factors produce the symmetry of the mandibular inferior border?
11. FAB Cephalometric Analysis (Profile Measurement)
- What does FAB stand for?
- What are common cephalometric errors that go unnoticed?
- What requirements are necessary for an accurate lateral head film?
- What are the natural head position and true vertical line?
- Can the profile projections be measured?
- What are the normal heights of the maxilla and mandible?
12. FAB Cephalometric VTO (Profile Treatment)
- Can a balance profile be built with numbers as part of bite correction?
- Can dental and skeletal factors be changed during bite correction to produce a balanced profile and a normal airway?
- What are the 7 steps involved in the VTO?
- Is the upper incisor position important to profile planning?
- What are the criteria for only operating the lower jaw?
- Should the base of the nose be retracted? Why not?
- What is facial harmony? Can it be measured?
13. Model Analysis (Bite Analysis)
- What is the model analysis form?
- What eliminates orthodontic relapse on surgical cases?
- How does model analysis determine maxillary expansion stability?
- What is the protocol for stable LFI expansion?
- What 3 factors lead to orthodontic bite correction relapse?
- How is tooth mass important to bite correction?
- What are the Multisegment LFI patterns?
14. Orthodontic Preparation - Part 1
- What are the 3 goals of orthodontic preparation?
- What are the keys to orthodontic tooth movement stability?
- Why does orthodontic tooth movement relapse with flat cusps?
- When should buccal cusps be bonded before surgery?
- What are the rules for surgical orthodontic preparation?
- Why does the upper first molar require orthodontic bands, headgear tubes, and lingual cleats for surgery?
15. Orthodontic Preparation - Part 2
- What is a one slide summary of excellent orthodontic preparation for surgery?
- What are the rules of presurgical equilibration? Why?
- Why is a Multisegment LFI utilized rather than a one piece?
- What is the literature regarding orthodontic relapse?
- What is postsurgical orthodontic retention?
- Regarding surgical and orthodontic tooth movements, why are teeth with cusps stable and teeth without cusps unstable?
16. Intermediate Splint
- Why operate the mandible first?
- How does the intermediate splint form guide model block or computer surgery?
- If a model block is used, what is the problem with opening the articulator pin?
- Is operating the mandible first more accurate and why?
17. Taking Records
- How are the wax bite and photographs accurately achieved?
- If the CR wax bite touches soft tissue, why is it inaccurate?
- How are cephalometric X-Rays developed accurately?
- Is a CBCT cephalometric X-Ray more accurate than a standard Ceph?
- How are natural head position (NHP) and true vertical line (TVL) determined?
- How is the CBCT volume oriented in the computer environment?
18. CBCT Orientation
- How is the CBCT volume oriented in the computer environment?
- Are the orbital rims leveled?
- Is the foramen magnum bisected?
- What variables control the symmetry of the inferior border of the mandible?
19. Hands On - Facial Measurement
- Is facial examination from photographs or directly on the patient?
- What is the form used for facial planning?
- Is facial planning an important part of bite correction?
- What 4 factors determine upper incisor exposure?
- How is a ruler used to determine canine canting?
- What does a history of extractions, headgear, and class II elastic tell us about upper incisor projection?
- What is facial quality versus position of facial parts?
20. Hands On – 2D and 3D FAB Part 1
- Do the maxillary midline, maxillary canines, and yaw orient the CBCT volume?
- Is the goal of orientation to have the volume represent the actual patient?
- Is the CBCT ceph more accurate than a standard ceph?
- What is the Arnett soft tissue cephalometric analysis (STCA)?
- What is the 7 step cephalometric treatment planning (CTP) protocol?
- Does the Arnett cephalometric treatment plan idealize the face, airway, and bite?
21. Hands On – 2D and 3D FAB – Part 2
- Why is the upper model so important?
- How many landmarks are used to orient the volume?
- How are the midline, cant and yaw set?
- Do I level the patient to the orbits or the canines?
- What type of BSSO splits are the best? And Why?
Videos / Chapters
SCREENSHOTS FROM THE COURSE